No Shame in Bedwetting: Tips and Ways to Handle it
2022-09-16 2022-09-16 18:04No Shame in Bedwetting: Tips and Ways to Handle it

No Shame in Bedwetting: Tips and Ways to Handle it
Bedwetting is a common problem in both young children and elderly teenagers and adults. Bedwetting can cause several issues, including embarrassment, discomfort, and upset. Besides that, bedwetters run the risk of aggravating damage to the skin by lying in a bed that is wet or soiled bed. Bedwetting is therefore an issue that needs to be resolved rather than simply accepting it as a fact.
Bedwetting could be reduced or eliminated in both children and adults by taking the necessary precautions. In essence, bedwetting, also known as nocturnal enuresis, is quite prevalent among young children, impacting approximately 5 million children in the United States. Bedwetting is defined as unplanned urination during sleep in children above the age of five.

Bedwetting can be a major issue for families. The important thing is that bedwetting is frequently a normal part of childhood development, and children usually develop out of it. It is typical for children to wet the bed during the toilet training years, even on a nightly basis. Bedwetting continues to remain frequent in children as young as five years old. It may also last into adolescence for some children.
A bedwetting child is unable to recognize and react to the feeling of a full bladder. Controlling bladder role while sleeping is a complicated system, and the age upon which your kid can do so varies. Approximately 20 percent of 5-year-olds, 10 percent of 7-year-olds, and 5 percent of 10-year-olds could still wet the bed.
How then do you realize if there's a concern?
According to the National Sleep Foundation, bedwetting is generally not seen as an issue until the child reaches the age of seven. If your child’s bedwetting continues after this age and he or she wets the bed more than 2 to 3 times each month, consult your pediatrician. Any inherent health issues must be ruled out by your pediatrician. Secondary bedwetting, for example, can be influenced by bloating or a urinary tract infection. Deep sleep, a small bladder capacity, increased night-time urine production, family background, and mental distress are all possible reasons for bedwetting. A few physicians will recommend bedwetting treatment as a final solution.
Why do children wet the bed?
In several instances, bedwetting is a hereditary issue passed down from a parent, aunt, or uncle. Because most grown-up children who wet the bed sleep very well, the signals of a build-up bladder are not solid enough to wake them. Some children have small bladders or do not generate sufficient vasopressin, a hormone that lessens urine production while sleeping. Bedwetting can be caused by anxiety and also significant progress in the family, such as a newborn baby or a distinct bedtime routine while on holiday.
Bedwetting could be an indication of some other medical condition in certain instances, particularly if it is a recent phenomenon.
Consult your pediatrician if your child is older than seven and has begun wetting the bed after being dry for several months. Your child’s primary care doctor will inquire about any hectic happenings or shifts in your child’s life and would monitor for ailments including diabetes, constipation, or a urinary tract infection. You may only perceive bedwetting as an issue if your child has it, such as if they are upset, or if there’s a health reason to be concerned. The child’s inspiration to end bedwetting must come from within.
How can parents assist a child who wets the bed?
The essential factor is not to hold responsible or disgrace your child as said by Kirk. Instead, he urges all to focus on intrinsic motivation and concrete actions you can take together. These tips and ways include;
Control your hydration levels and urination during the day
Pay attention to what’s happening during the day. What occurs at night is affected by the scheduling of hydration and urination during the day. Work with your child to establish the routine of peeing every 2 or 3 hours, even if they do not have the urgency. Allow them to urinate two times before sleeping: once an hour before bed and again shortly before bedtime. Use a calendar tracking service to help your child comprehend peeing trends as they progress. CHOP’s website features two of these tracking systems, one for children and young teenagers and one for adolescents. it can aid your child take control over their bedwetting and see and feel positive about their advancement. Instead of waiting until the end of the day to suppress their thirst, motivate them to consume plenty of fluids early in the day. Children who play games close to the end of the day should drink water before their training or sport, and afterward, make effort to reduce their intake of water in the evening.
Look into getting a bedwetting alarm
Bedwetting alarms sound when urine is detected in the middle of the night, effectively training adults and children to correlate the feeling of a build-up of fluid in the bladder with getting up and using the bathroom. The technique is quite efficient when used continuously over a lengthy period.
A moisture sensor in bedwetting alarms activates a bell or buzzer when the child’s pajamas become wet. “Initially, the alarm is for the caregiver,” Kirk explains. “If a child could sleep throughout the night in a wet bed, he or she will sleep through the alarm.” As a result, you should consider installing a baby monitor in the child’s room. It takes a while, but most children though not all, learn to awaken after 3 or 4 months to visit the washroom.
Discuss treatment with your child's primary care physician
Some children benefit from DDAVP®, or desmopressin, a drug administered as a pill before going to bed to decrease the quantity of urine produced during sleep. When utilized in combination with fluid and forfeiting administration during the day, DDAVP can be a useful resource for important activities such as sleepovers and sleep-away camps.
Reduce your caffeine intake
Caffeine has been proven to significantly raise urine production, so it is advised to limit your consumption of caffeine-containing beverages like coffee, tea, carbonated drinks, energy drinks, and cocoa, particularly shortly before bedtime.
Visit the washroom before going to bed
Make sure there is convenience and accessibility to the bathroom. It might be as easy as accessing the bathroom on time, especially for several bedwetters. This is particularly common when working with young children, impaired or grown-ups, or mentally challenged people.
The following are some suggestions for making nighttime toileting secure and simpler: Make the path between the bed and the bathroom clear to avert slips and falls, Utilize artificial lighting to aid your adored one in quickly finding the bathroom, and put in place an elevated toilet seat to make it simpler for adults with impaired mobility to use the bathroom autonomously.
Keep track of bowel movements
Bloating can impede efficient bladder emptying, so keep an eye on bowel movements to be certain your adored one isn’t experiencing pain needlessly. If bloating or abnormalities are presumed, talk to your physician about the ideal method to treat the problem and prevent unnecessary overnight spills.
Wearable safeguarding
Wearable safeguarding including baby diapers, teenagers or adult diapers, and water-absorbing underwear, also widely recognized as pull-ups, could effectively safeguard your cherished one’s skin and beds conveniently dry all through the night until they are taught or successfully treated for their bedwetting problems. Expendable incontinence merchandise, particularly those intended for night-time use, can hold a significant volume of liquid and are simply discarded when soiled.
Bedding safeguarding
When wearable safeguarding is not enough to maintain the napkins dry during the night, bed pads can effectively safeguard the part of the bed that is most highly probable to get wet or soiled.
To reduce washing after an incident occurred of wetting, consider buying cost-effective and environmentally friendly recyclable under pads or easily expendable bed chucks with dependable permeability and water-resistant support.
Mattress safeguarding
Mattress covers and mattress pads will not keep your bedding dry, but they will safeguard your mattresses from urine harm and are an essential step to recognize if your cherished one has bedwetting problems. These merchandises are water-resistant and generally simple to keep clean, and they provide dependable protection that allows for a longer mattress life. Remember that while denser mattress pads offer greater solace for the owner, the depth furthermore implies that cleaning and drying these pads would then take a while longer.
Conclusion
Bedwetting can be challenging and aggravating for any caregiver, it is however essential to keep the incapacitated person’s emotions as well. Very often resist taunting, accusing, or disciplining dearest ones who have bedwetting problems. The latter initiative would not only be ineffectual because the issue is beyond the child’s or adult’s influence; it may even worsen the situation. Rather, concentrate on uplifting and assisting your cherished one during this tough period, and you’ll be quite well in your direction to dry, anxiety-free nights becoming the new reality.
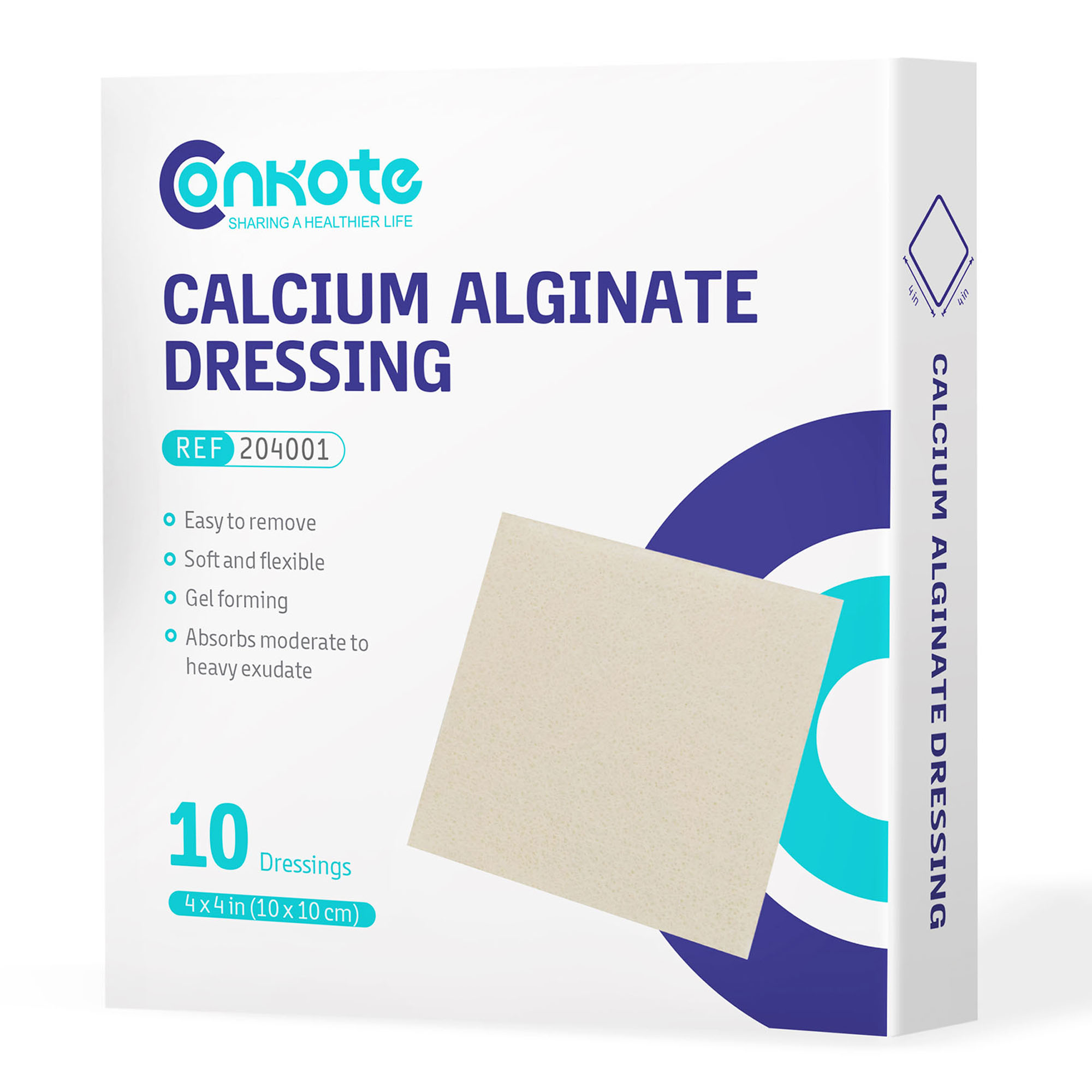
Search by Tags
advanced woundcare dressing advanced wound care products Bedsores Blood Blood donation chronic decrease comprehensive guide Conkosil Conkote wound care Diabetes diabetes prevention Diabetes,Foot Problems,wound donation Easy Tips elderly skin care First aid fragile skin dressing gentle wound dressing health life Home Care Ionic Silver Dressin Innovative Technology for Wound Care Lesions Measure a Wound medical tape medical tape for sensitive skin Moist Wound Healing Mouth Taping Negative pressure wound therapy Pressure Ulcers Self-Adhesive Bandage senior wound care silicone foam dressing silicone medical tape Skin care tape traditional wound care dressing Wound care wound care for elderly wound dressing wound healing wound infection wound materials woundmaterials wound type wound vac