Diabetic Foot Ulcers – Symptoms, Causes, Treatment and Care.
2022-03-01 2022-06-23 18:05Diabetic Foot Ulcers – Symptoms, Causes, Treatment and Care.

Diabetic Foot Ulcers – Symptoms, Causes, Treatment and Care.
Diabetes is the leading cause of nontraumatic lower extremity amputations in the United States, and approximately 14 to 24 percent of patients with diabetes who develop a foot ulcer have an amputation. However, has shown that the development of a foot ulcer is preventable.
Diabetic foot is a complication of diabetes, which usually occurs in the feet of patients. How much do you know about diabetic foot?
0:No open lesions; may have healed lesion.
I: Superficial ulcer without penetration to deeper layers.
II:Deeper ulcer, reaching tendon, bone, or joint capsule.
III:Deeper tissues involved, with abscess, osteomyelitis, or tendonitis.
IV:Gangrene in a portion of forefoot or heel.
V:Extensive gangrenous involvement of the entire foot.

Ulcers in people with diabetes are most commonly caused by:
- Poor circulation
- High blood sugar (hyperglycemia)
- Nerve damage
- Irritated or wounded feet
Who gets diabetic foot ulcer?
Anyone with diabetes can develop foot ulcers. Native American, African American, Hispanic, and older men are more likely to develop ulcers. People who use insulin have a higher risk of foot ulcers, as do people with diabetes-related kidney, eye and heart disease. Being overweight and using alcohol and tobacco also play a role in the development of foot ulcers.

Preventing diabetic foot ulcers:
1. Optimizing diabetes control to reduce neurological and vascular complications.
2. Quit smoking.
3. Regularly check at-risk feet and carefully trim toenails.
4. Prompt treatment of non-ulcer conditions such as tinea pedis or cracked heels.
5. Appropriate footwear.
6. Exercise and physical therapy.
7. Education of patients, families, and healthcare providers.
Treatment. The key to successful wound healing is regular podiatric medical care to ensure the following “gold standard” of care:
1. Managing blood glucose and other health problems.
2. Multidisciplinary care – may include endocrinologist, podiatrist, diabetes education nurse, wound care nurse, neurologist, vascular surgeon and/or orthopaedic surgeon.
3. Taking the pressure off the area, called “off-loading”.
4. Removing dead skin and tissue, called “debridement”.
5. Applying medication or dressings to the ulcer.
6. Prevent secondary infection.

Specific measures
1. Treatment of secondary infection.
2. Ulcer debridement.
3. Dressings.
4. Adjuvant therapies — negative pressure wound therapy, ulcer excision and grafting, topical or hyperbaric oxygen, human growth factors, or amputation.
What is the outcome for diabetic foot ulcer?
Diabetic foot ulcer may:
Heal over weeks to months.
Re-ulcerate — recurrence rate is 40% within one year, 60% by three years, and 65% at five years.
Result in lower extremity amputation in 14–24%.
The five-year mortality rate has been estimated to be 42%.
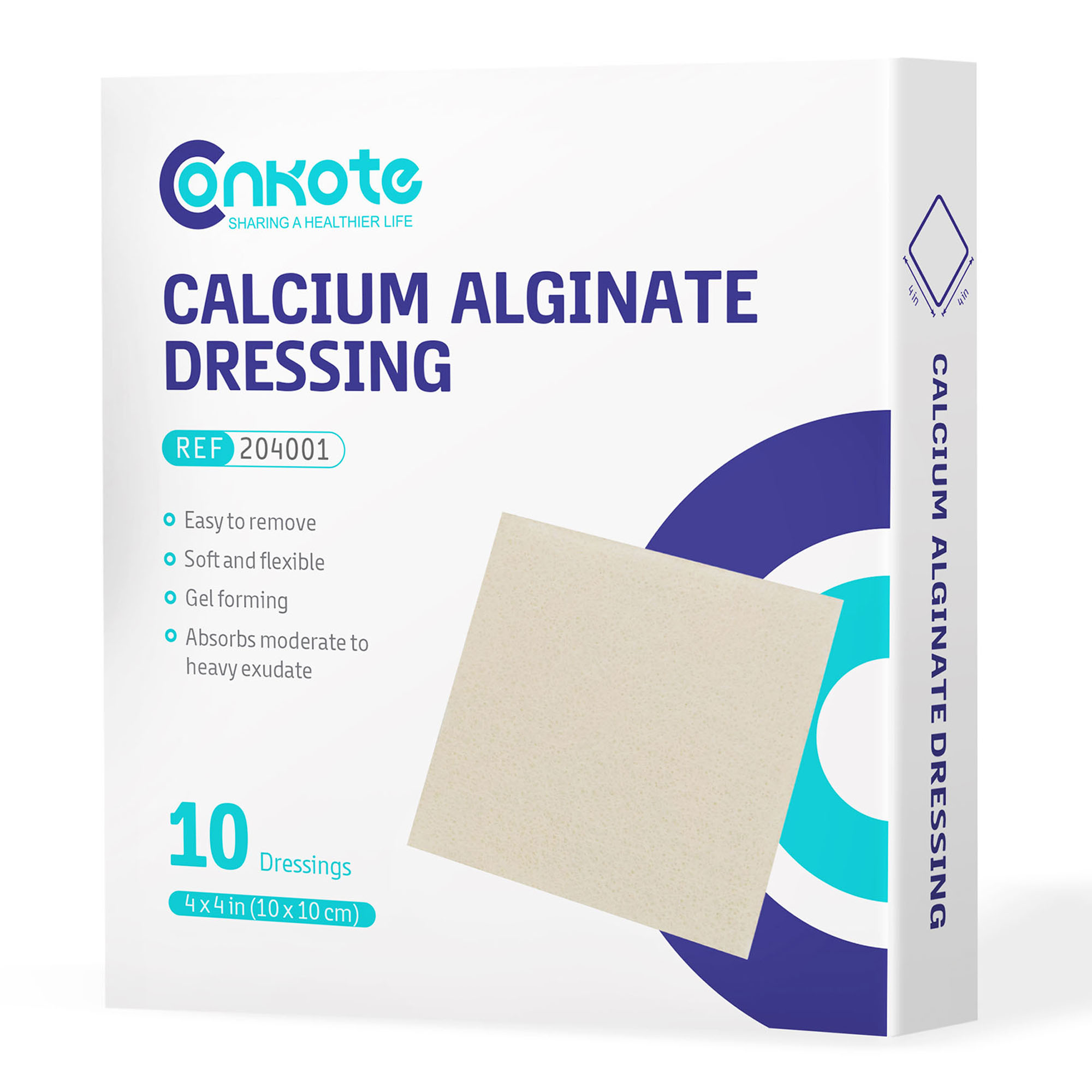
Appropriate wound management includes the use of dressings and topical medications. These products range from saline to advanced products such as dressings that have been shown to be very effective in healing foot ulcers.
Choose Conkote Foam Dressing with Silicone Adhesive Border:
Foam dressing with silicone layer is manufactured with foam, silicone layer, PU film, and isolation film. The soft and flexible foam absorbs large amount exudates, reduces risk of maceration, silicone adhesive border provided gentle and safe fixation, makes the dressing to remove easily with no pain. It is indicated for a wide range of moderate to highly exuding wounds.

Healing time depends on factors such as wound size and location, pressure on the wound fromwalking or standing, swelling, circulation, blood sugar levels, wound care, and application on the wound. Healing may occur within weeks or months. Don’t know how to choose the right dressing? Check Conkote® Wound Dressing Selection: Types and Usage
What is a healthy, balanced diet for diabetes?Your food choices matter a lot when you’ve got diabetes.
Starches: Whole grains, such as brown rice, oatmeal, quinoa, millet, or amaranth. Baked sweet potato. Items made with whole grains and no (or very little) added sugar.
Vegetables: Fresh veggies, eaten raw or lightly steamed, roasted, or grilled. Plain frozen vegetables, lightly steamed. Greens such as kale, spinach, and arugula. Iceberg lettuce is not as great because it’s low in nutrients. Low sodium or unsalted canned vegetables.
Fruits: Fresh fruit. Plain frozen fruit or fruit canned without added sugar. Sugar-free or low-sugar jam or preserves. No-sugar-added applesauce.

Reference materials:
https://www.webmd.com/diabetes/diabetic-food-list-best-worst-foods
https://www.medicalnewstoday.com/articles/317504#complications