Diabetes Foot Problems: How to Prevent Related Amputations?
2024-05-06 2024-05-06 18:16Diabetes Foot Problems: How to Prevent Related Amputations?

Diabetes Foot Problems: How to Prevent Related Amputations?
Diabetes is a chronic (long-lasting) disease that affects how your body turns food into energy. Diabetic foot refers to infection, ulceration or destruction of tissue in the foot of a diabetic patient. It is usually associated with lower extremity neuropathy or peripheral arterial disease.
Diabetic foot ulcer is the most common clinical manifestation of diabetic foot patients, and it is also one of the important reasons leading to amputation in diabetic patients.
How Does Diabetes Cause Foot Problems?
Foot problems are common in people with diabetes. They occur over time when high blood sugar damages the nerves and blood vessels in the feet. This nerve damage, called diabetic neuropathy, can cause numbness, tingling, pain, or loss of feeling in the feet.
If you can’t feel pain, you may not know you have a cut, blister, or ulcer (open sore) on your foot. A wound like that can become infected. The infection may not heal well because damaged blood vessels can cause poor blood flow to the feet.
Infection and poor blood flow can lead to gangrene. This means muscle, skin and other tissues start to die. If your gangrene or foot ulcer does not get better with treatment, you may need Lower-limb amputations(LLA). This is surgery to remove a damaged toe, foot, or part of a leg. It may prevent a bad infection from spreading and could save your life.
How Diabetes Can Lead to an LLA?
Lower Limb Amputation (LLA) is increasing in the United States, 80% of which are the result of complications from diabetes.
High blood sugar over time can cause diabetes complications that raise the chance of an LLA:
- Peripheral arterial disease (PAD)can narrow the blood vessels that carry blood to your legs and feet. Poor blood supply can make even a tiny cut heal slowly or not at all.
- Peripheral nerve damagecan cause loss of sensation so you may not notice cuts, sores, or ulcers on your feet.
With these complications, even a small cut can become a serious infection. Depending on the condition, a doctor may recommend:
- Procedure to clean the wound and remove dead tissue.
- Surgery to restore blood flow to your leg or foot (called revascularization).
- Antibiotics to treat certain infections.
- Amputation to remove the affected area.
When to See Your Doctor?
There are many things to manage if you have diabetes: checking your blood sugar, find time to be active, make healthy foods, take medicines on time, see the doctor. Other than that, your most important thing – care about your feet.
A small wound on the foot can turn into a serious infection that may require amputation if left untreated.
Check your feet every day, so you can catch any foot problems early and treat them right away. Early treatment can greatly cope with challenges, and prevent diabetes complications like LLAs.
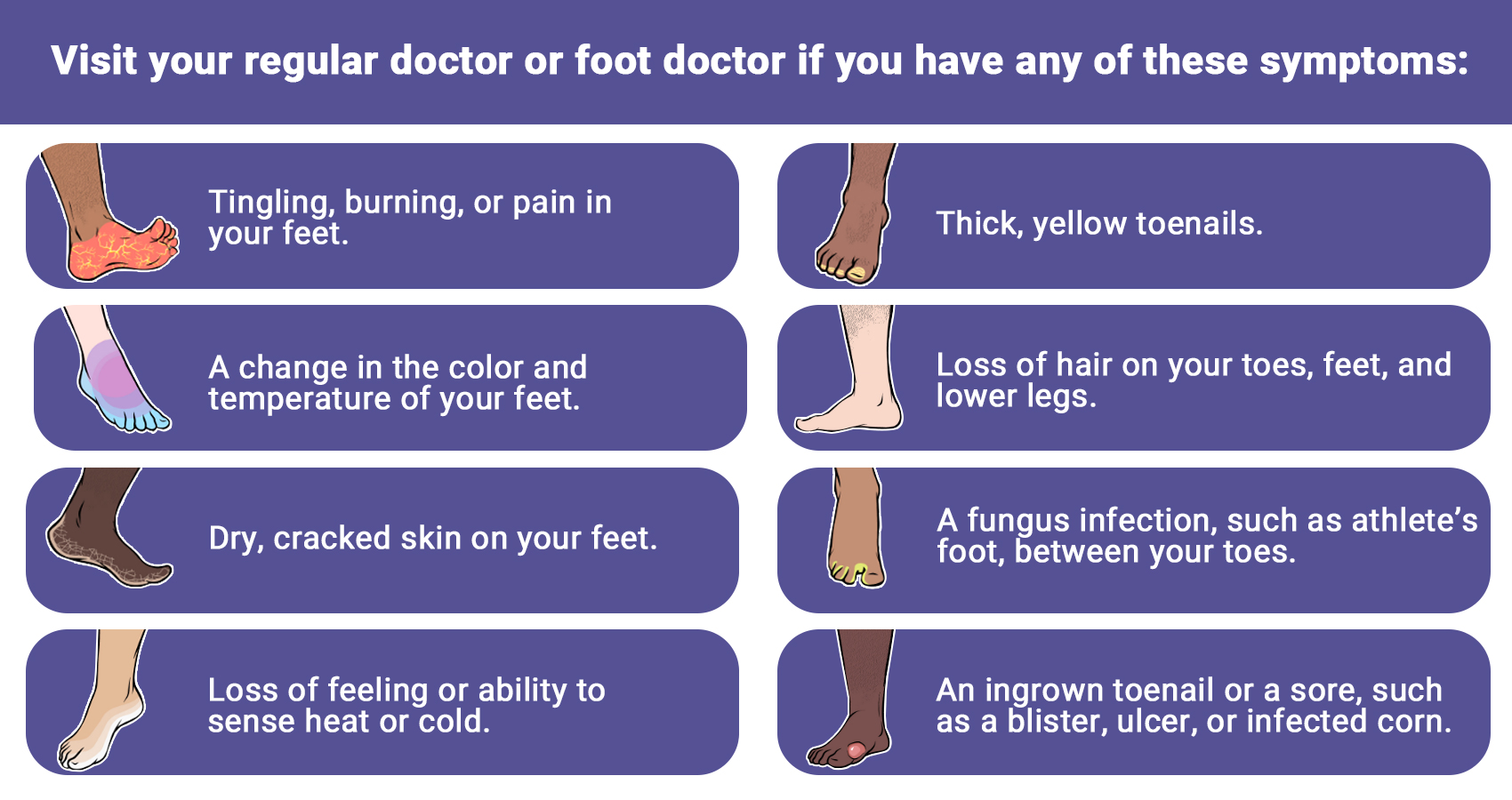
If you have any of the following symptoms, don’t wait until it becomes a serious infection. See your primary doctor or foot doctor right away if:
How Can Protect Diabetes Foot ?

The best way to protect your feet is to control your blood sugar levels in daily life. This will help prevent nerve and blood vessel damage from getting worse. The next step is to keep the skin on your feet healthy.
Good foot care for people with diabetes includes:
- Checking your feet every day. Look for cuts, redness, and other changes in the skin and toenails, including warts or other spots that your shoes could rub. Make sure to check the bottoms of your feet too.
- Washing your feet every day. Use warm water and soap. Don’t soak your feet because that can dry out your skin. After you dry your feet, you can use talcum powder or cornstarch between your toes. They soak up moisture that can cause infection. If you use lotion, don’t apply it between your toes.
- Asking your doctor how to remove corns and calluses safely. Thick skin on your feet can rub and lead to sores. But removing it the wrong way could damage your skin. So you don’t want to cut the skin or use medicated pads or liquid removers.
- Trimming your toenails straight across with a clipper. If it’s hard for you to trim your own toenails, or if they’re thick or curve into the skin, have a podiatrist (foot doctor) do it for you.
- Always wearing well-fitting shoes and socks or slippers to protect your feet when walking. You don’t want to walk barefoot, even indoors. And be sure your shoes are smooth inside. A seam or pebble could rub your skin raw.
- Protecting your feet from heat and cold. Use sunscreen on exposed skin and don’t walk barefoot at the beach. In cold weather, wear warm socks instead of warming your feet near a heater or fireplace.
- Keeping the blood flowing in your feet. Put your feet up when you’re sitting. Wiggle your toes and circle your feet throughout the day. Don’t wear tight socks. And get plenty of activity that’s not too hard on the feet, such as walking.
- Getting your feet checked at your health care visits. Even if you haven’t noticed a problem, it’s good to have your health care provider look at your feet.
Wound treatment is an important part of diabetic foot ulcer management, and dressing is one of the main tools.
The International Working Group on the Diabetic Foot(IWGDF) recommends choosing an appropriate dressing to control exudation and infection, maintain a moist environment, and promote ulcer healing.
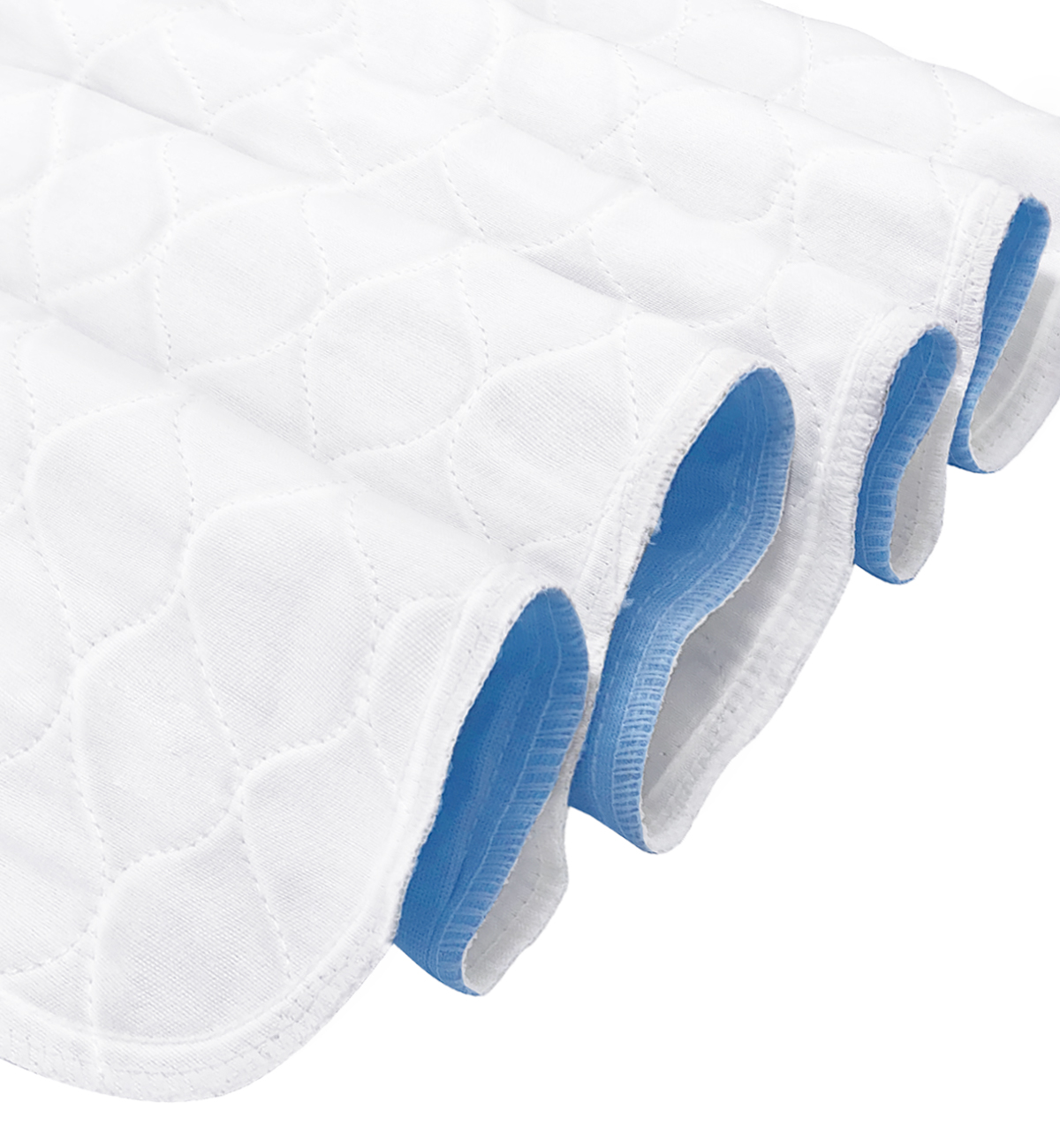
Conkote Foam Dressing with Silicone Adhesive Border
- Silicone layer foam dressing is made of foam, silicone layer, PU film and isolation film.
It maintains a healthy moisture environment, forms a barrier from the outside world, and promotes wound healing.
- Medical grade hypoallergenic soft silicone is used as the wound contact layer. It absorbs dead tissue cells without sticking to wet wounds, minimizing pain and trauma during dressing changes.
Choosing appropriate dressing for your needs can promote healing and reduce pain.
If you want to learn more about silicone foam dressing, check out: https://store.conkote.com/product/conkote-ultra-absorbent-silicone-foam-dressing-with-border/
Conclusion
As one of the most serious complications of diabetes, diabetic foot is also one of the main causes of disability and death due to diabetes. With the increasing trend of complications, this will arouse the attention of all of us. Diabetic patients should carefully observe their feet every night before going to bed to check whether there are ulcers, redness and swelling on the skin surface of the feet. If abnormalities are found, they should be dealt with in time, or go to the hospital to listen to the doctor’s advice .
Search by Tags
advanced woundcare dressing advanced wound care products Bedsores Blood Blood donation chronic decrease comprehensive guide Conkosil Conkote wound care Diabetes diabetes prevention Diabetes,Foot Problems,wound donation Easy Tips elderly skin care First aid fragile skin dressing gentle wound dressing health life Home Care Ionic Silver Dressin Innovative Technology for Wound Care Lesions Measure a Wound medical tape medical tape for sensitive skin Moist Wound Healing Mouth Taping Negative pressure wound therapy Pressure Ulcers Self-Adhesive Bandage senior wound care silicone foam dressing silicone medical tape Skin care tape traditional wound care dressing Wound care wound care for elderly wound dressing wound healing wound infection wound materials woundmaterials wound type wound vac