Chronic Wounds 101: Causes, Types, and Treatment
2022-08-05 2022-08-19 11:09Chronic Wounds 101: Causes, Types, and Treatment
Chronic Wounds 101: Causes, Types, and Treatment
Every day, most people go about their business without incident. Unfortunately, sometimes injuries occur. In most cases, these injuries result in minor, acute wounds that heal within a few days or weeks, but sometimes they are more serious. When acute wounds do not heal properly or become infected, they result in chronic injuries. Wounds become chronic when they do not progress through the predictable rate of healing.
If a wound takes over four weeks to heal after treatment, it is considered chronic. When healing takes longer than two weeks, the wound is more serious and requires proper care to avoid further problems. In this article, we will discuss how to care for chronic wounds and what to do when complications occur.
What is a Chronic Wound?
Wound chronicity refers to the physiological deterioration of wounds caused by a disruption in the wound healing cascade. Infection is the most common cause of delayed healing of chronic wounds. For effective treatment of chronic wounds, it is essential to understand the normal healing process and wound bed preparation (WBP). Chronic wounds result from impaired blood flow, neuronal stimulation, or cellular migration.
The normal healing process for wounds comprises four distinct phases. Wounds begin with hemostasis, which is the process of clotting that occurs immediately after an injury. Hemostasis protects your body from bleeding and helps start the healing process. Some medical conditions may interfere with hemostasis, so talk to your doctor if you have diabetes or another chronic illness.

Next, inflammation occurs. During this time, the body signals the cells to protect the injury site. An acute wound differs from a chronic wound in that inflammation happens during healing. As soon as inflammation occurs in an acute wound, proliferation begins. In chronic wounds, inflammation continues, and the wound does not heal. In some cases, your body cannot activate tissue cells and fight infection, so the wound worsens. Call your doctor immediately to avoid serious complications if you suspect you have an infected wound.
Causes of Chronic Wounds
A variety of factors can cause chronic wounds, including increased bacterial load, inadequate blood supply, infection, and improper treatment. Traumatic injuries can also result in chronic wounds. Monitoring your wounds is essential to preventing chronic wounds. Other causes of chronic wounds include:
- Smoking
- Poor Nutrition
- Obesity
- Reopening surgical wounds or ripped stitches
- Ulcers caused by excessive pressure on the skin
- Circulation problems: ulcers on the feet or legs
- Diabetic ulcers
- Bacterial infections
Common Chronic Wounds
Assessing a patient’s wound is necessary to determine if it will become chronic. Those with multiple comorbid conditions, such as diabetes or obesity, are more likely to experience delayed healing. Chronic wounds can also occur in patients who take certain medications or smoke. Some chronic wounds include:
- Venous ulcers – Venous ulcers occur when vein valves malfunction and allow blood to pool in the veins, resulting in swelling and ulcer development.
- Arterial ulcers –Arterial ulcers occur when there is not enough nutrient-rich blood flowing to the lower extremities, resulting in oxygen-deprived tissue being damaged.
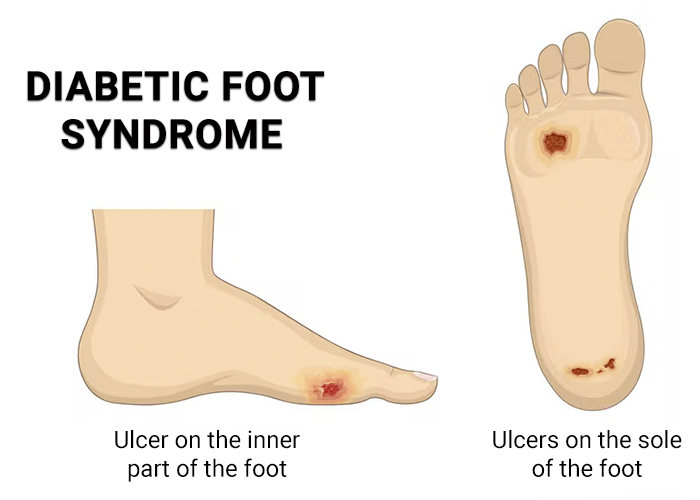
- Diabetic foot ulcers –Diabetic foot ulcers develop as a result of repetitive trauma to the foot, usually over deformed areas or in patients with neuropathy. This reduces sensation in the foot.
- Pressure injuries –Pressure injuries can develop over bony prominences after prolonged pressure or friction.
When it comes to assessing a patient with chronic wounds, a holistic approach is best. Comprehensive treatment plans involve wound assessment, a thorough medical history, physical examination, wound assessment, nutritional status, and self-care status. In some cases, it can be difficult to determine the wound’s etiology.
Traumatic or surgical wounds, radiation injuries, and malignancies can all become chronic under the right conditions. Diabetes, obesity, autoimmune disease, medications, peripheral arterial disease, and anatomical location all contribute to wound chronicity and infection risk.
The most common chronic wound conditions
Diabetes
Chronic wounds are most often associated with diabetes. Diabetic patients are more likely to develop foot ulcers than nondiabetics due to changes in blood vessels, nerves, and skin. This is usually caused by peripheral neuropathy, or a loss of sensation in your feet, making it difficult to notice wounds after stepping on a sharp object or developing blisters immediately.
Diabetes patients should check their feet regularly for wounds and changes in the skin. Ideally, diabetic patients should wear footwear designed specifically for their feet. By wearing these shoes, you can reduce irritation and protect your feet from foreign objects. To help keep the skin moist, flexible, and resistant to tears, use a lotion designed specifically for diabetic patients.
Check this blog to know more about diabetes foot: Diabetic Foot Ulcers – Symptoms, Causes, Treatment and Care
Limited Mobility
occur when the skin presses against a hard surface for an extended period. In this area, if blood flow is reduced, tissues can be damaged or die, resulting in ulcers.
Abrasions should be checked regularly to ensure they are healing properly to minimize the risk. In order to prevent pressure ulcers, a mobility expert or doctor may recommend padding, cushions, or a rotation routine. The spine and hips, which are frequently in contact with hard surfaces, require special attention.
Varicose Veins
In the United States., about 20 percent of adults suffer from varicose veins, which are twisted or swollen blood vessels that can cause chronic wounds or ulcers. Varicose veins cause tension, swelling, and skin disorders, like hemosiderin deposits, which weaken the skin and prevent wounds from healing. If you spend a lot of time sitting or standing, compression socks are often recommended to prevent varicose veins. Exercise, quitting smoking, and elevating your legs while resting can help.
Innovative treatments in wound care
Negative pressure wound therapy
Through the use of suction, excess fluid is removed from the wound. This revolutionary procedure is known as vacuum dressing. In order to create suction on a wound, a vacuum pump is attached to a sealed foam or gauze dressing. As well as removing excess fluid from the wound, suction can also help the wound’s edges come together and increase circulation to the area, which aids in natural wound healing. Treatment usually takes between one and two weeks, with weekly wound dressing changes
Biological dressings
Dressings made from biological materials serve as temporary covers for wounds, preventing fluid loss and protecting them from infection. Dressings are usually made from organic materials such as human stem cells or bovine collagen. Along with insulating the wound from the elements, the dressing can also activate the tissue surrounding the wound in a healing process. The recovery time will depend on the location and severity of the wound.
Vascular procedures
Chronic wounds stemming from blocked blood flow can also be surgically treated. It is possible to open blood vessels in the lower extremities by using minimally invasive procedures, such as stent placement and angioplasty. A catheter, a thin, flexible tube, is used to enter the patient’s blood vessel through the groin. A small balloon is inflated through the tube, and a stent is placed to keep the blocked vessel open. The recovery time length depends on the wound’s severity and the extent of the blockage.
Standard treatment
While wound care advances, standard treatments such as wound closure and skin grafting remain effective treatments. In most cases, debridement is required to provide a clean, smooth surface by removing dead or unhealthy skin. When the damaged skin is removed, the body is reminded to heal, and healing is accelerated.
Types of Wound Dressing
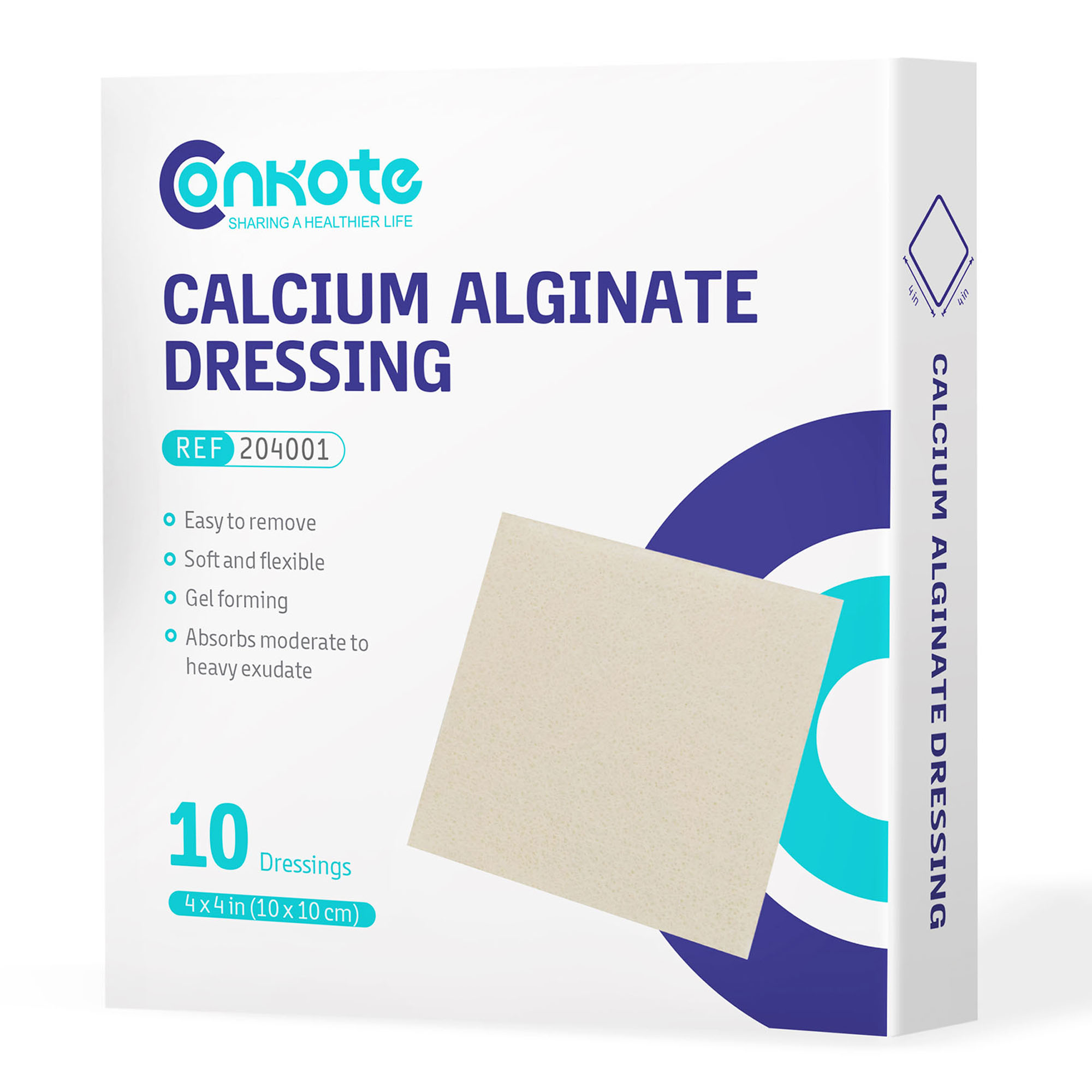
There is a range of foams and super absorbent dressings complemented with advanced wound dressings. Each dressing supports a specific wound healing process. Among the assortment are:
Designed for wounds that are exuding heavily, alginate binds calcium ions to the wound’s fluid. Alginate causes the fibers in the dressing to swell and partially dissolve into a gel. This dressing absorbs exudate and creates a moist wound environment.
Soft silicone dressings are suitable for a wide range of wounds, including venous leg ulcers, partial-thickness burns, traumatic wounds, and diabetic foot ulcers,
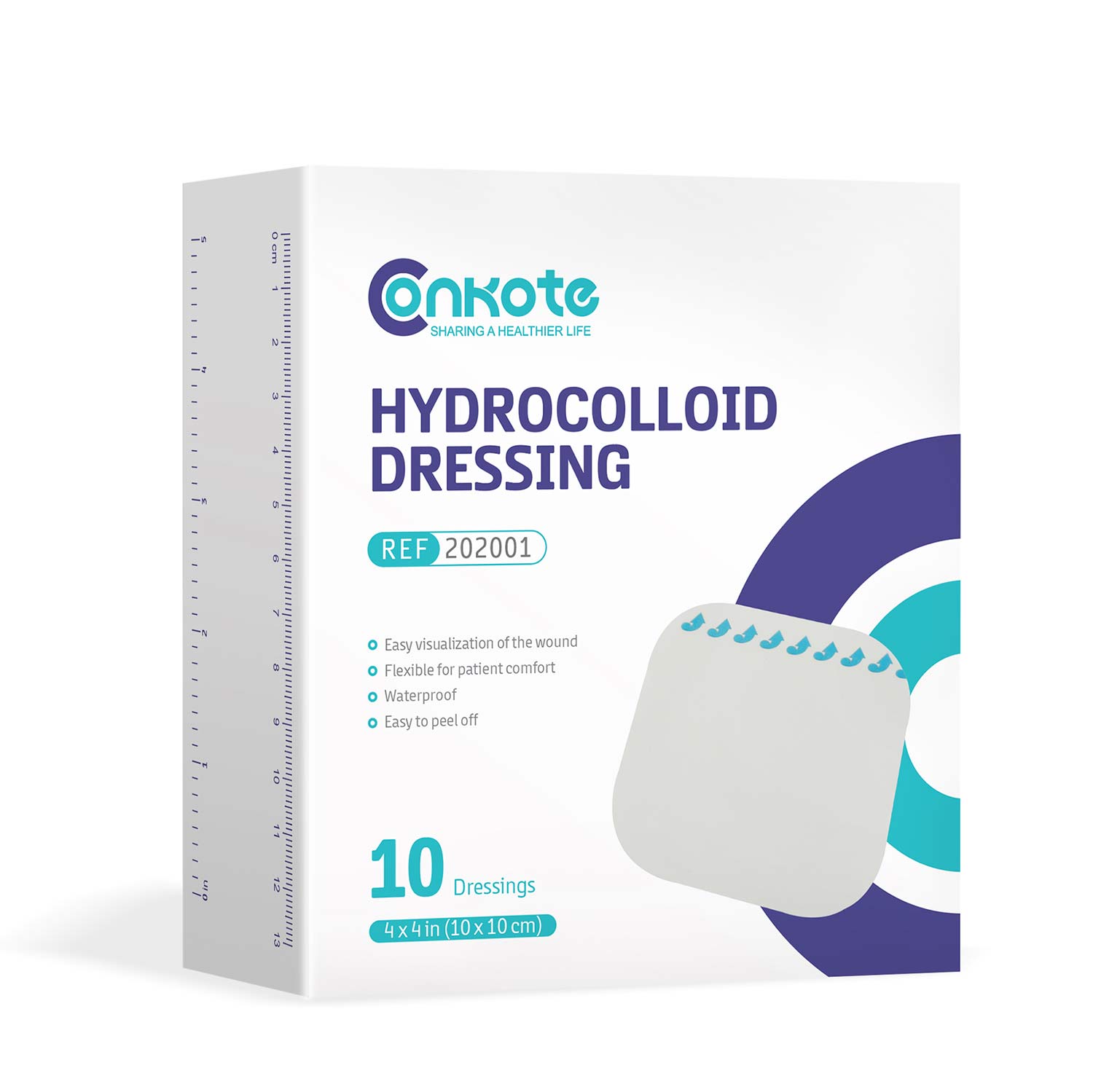
A hydrocolloid dressing provides a moist, insulating healing environment that protects uninfected wounds and allows the body’s enzymes to aid in healing. The dressings are unique because they do not need to be changed as often as some other wound dressings. They are also easy to use. The dressing consists of polyurethane foam coated with hydrocolloid and is self-adhesive. It is suitable for wounds with little exudate on the surface, and it can be used in conjunction with compression therapy.
Transparent films vary in thickness and size and are semipermeable polyurethane membranes. They are waterproof and impervious to bacteria and contaminants, yet they allow water vapor to pass through. Transparent Film promotes the formation of granulation tissue and the autolysis of necrotic tissue by maintaining a moist environment. As a primary or secondary dressing, transparent films can be used to prevent and manage pressure ulcers, partial thickness wounds without exudate, and wounds with necrotic tissue.
Conclusion
Chronic wounds must be adequately cared for if you want to avoid serious complications or infections. The best way to do this is always to keep wound care supplies and dressings on hand.
Search by Tags
advanced woundcare dressing Bedsores Blood Blood donation chronic decrease Chronic Wound comprehensive guide Conkosil Diabetes diabetes foot diabetes prevention Diabetes,Foot Problems,wound Diabetic foot dog training donation dor pee pads Easy Tips First aid health health life Home Care Ionic Silver Dressin Innovative Technology for Wound Care Lesions Measure a Wound medical tape Moist Wound Healing Negative pressure wound therapy papertape pet care Pressure Ulcers puppy pee pads Self-Adhesive Bandage Skin care tape Tobacco traditional wound care dressing World No Tobacco Day Wound care wound dressing wound healing wound infection wound materials woundmaterials wound type wound vac