Bedsores, Pressure Ulcers, Lesions: Name Them What You Want, But Know the Facts
2024-07-12 2024-07-12 14:59Bedsores, Pressure Ulcers, Lesions: Name Them What You Want, But Know the Facts

Bedsores, Pressure Ulcers, Lesions: Name Them What You Want, But Know the Facts
Many things in life have different names, and medicine is no exception. You might know these skin issues as bedsores, pressure ulcers, pressure sores, or simply sores. Regardless of the name, they’re essentially the same thing.
Understanding, recognizing, and preventing these sores is crucial for maintaining patient health. If your loved one already has one of these wounds, having the right knowledge is key to providing the best care and treatment.
Contrary to common belief, having a bedsore or pressure ulcer doesn’t mean it’s impossible to heal. Although the process can be challenging and requires careful attention from a healthcare professional, healing a sore is definitely achievable.
What Are Bedsores, Pressure Ulcers, or Sores?
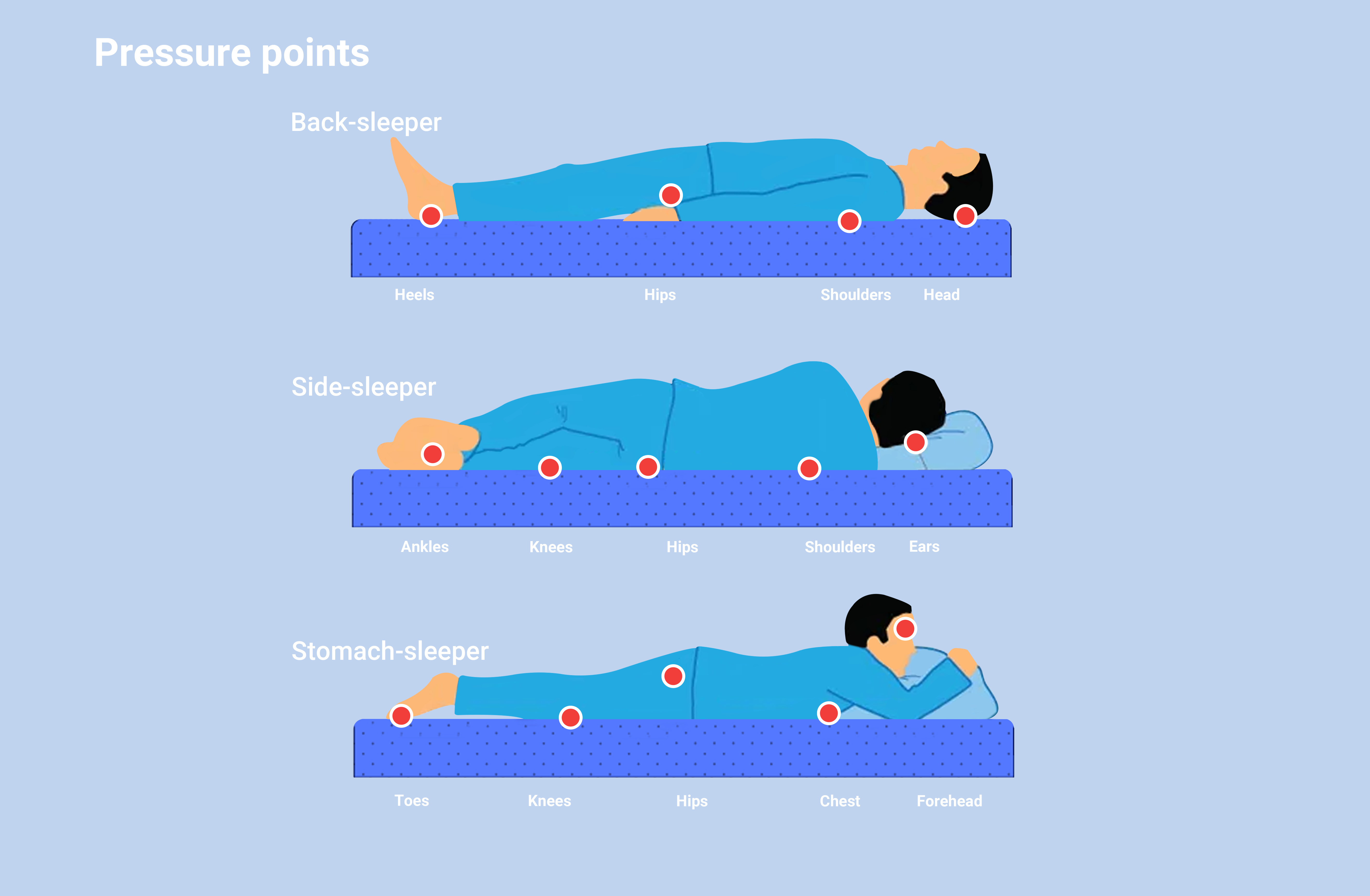
These are injuries to the skin and underlying tissue caused by prolonged pressure on the skin. They occur when someone stays in the same position for too long, leading to constant pressure on certain areas of the body.
These areas are usually bony parts like heels, elbows, hips, and the back. Continuous pressure cuts off blood flow to the skin and tissue, eventually causing the tissue to die and a sore to form.
Anyone can develop a pressure ulcer, regardless of age, gender, weight, or other health conditions.
How Do Pressure Ulcers Form?
Pressure ulcer can form quickly. They develop when blood flow to the skin is reduced or cut off due to pressure. This lack of blood flow can cause a pressure sore to develop in just two hours.
The outer layer of skin, the epidermis, begins to die. As dead cells break down, a pressure ulcer forms. Ulcers are more likely to develop when pressure is combined with:
- Moisture from sweat, urine, or feces.
- Shear and friction from sliding down in a tilted bed or wheelchair.
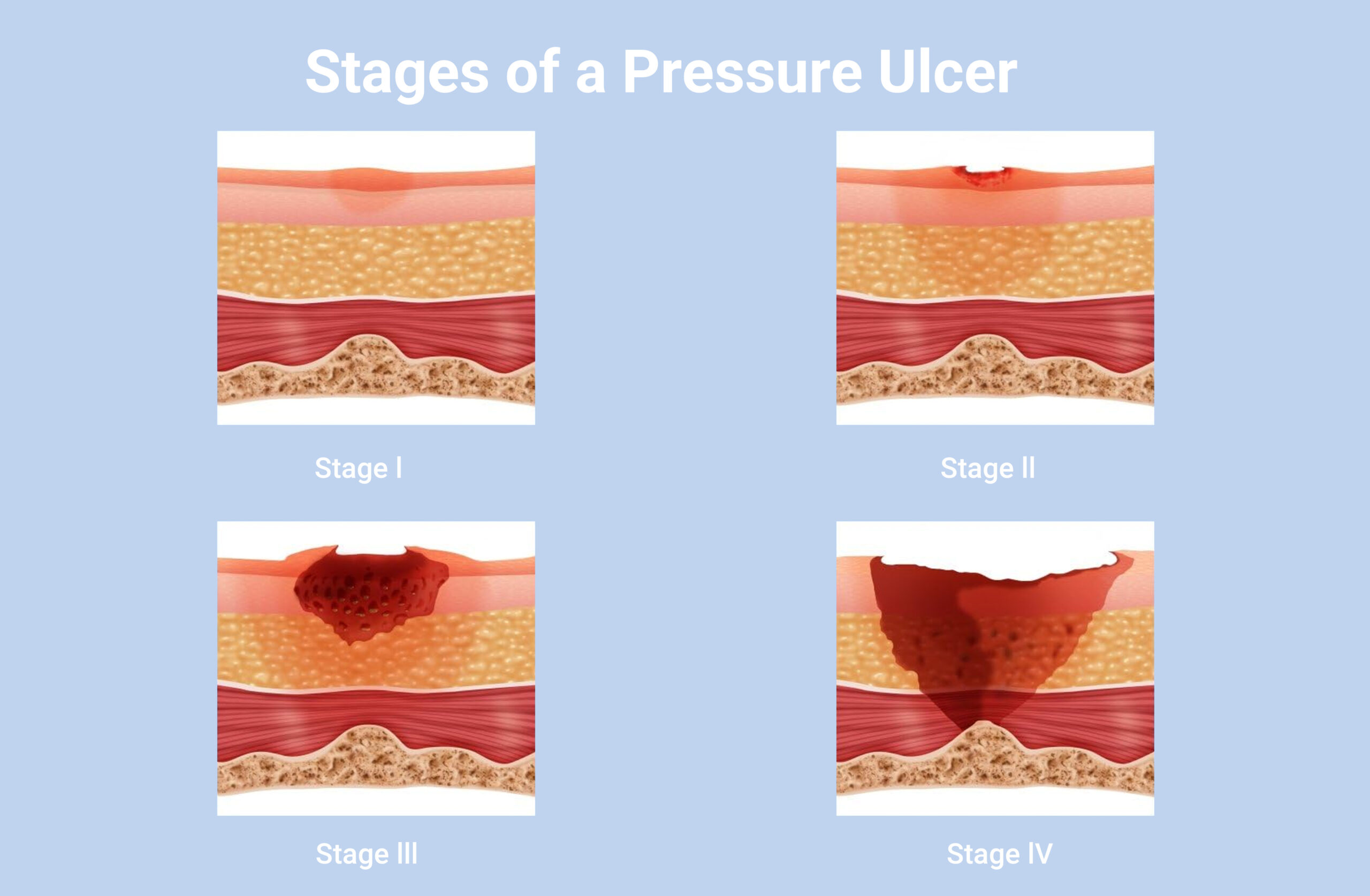
How to Recognize Pressure Ulcers
Recognizing a pressure ulcer early is essential for prompt treatment. Here’s what to look out for:
- Discolored patches of skinthat don’t change color when pressed. These patches are often red on lighter skin, or purple or blue on darker skin.
- Warm, spongy, or hard skin patches.
- Pain or itchingin the affected area.
- Ulcers usually develop gradually, but they can appear in a few hours.
Who Is at Risk for Pressure Ulcers?
People with thinner skin and those who have limited or no ability to move are more likely to develop pressure ulcers. This includes people who:
- Are in a coma or vegetative state.
- Are paralyzed.
- Use wheelchairs.
- Wear casts, splints, or prostheses.
Children and adults with certain health conditions are also more prone to developing sores. These conditions include:
- Cancer
- Cerebral palsy
- Chronic venous insufficiency
- Dementia
- Diabetes
- Heart failure
- Kidney failure
- Malnutrition
- Peripheral artery disease
- Spinal cord injury or spina bifida
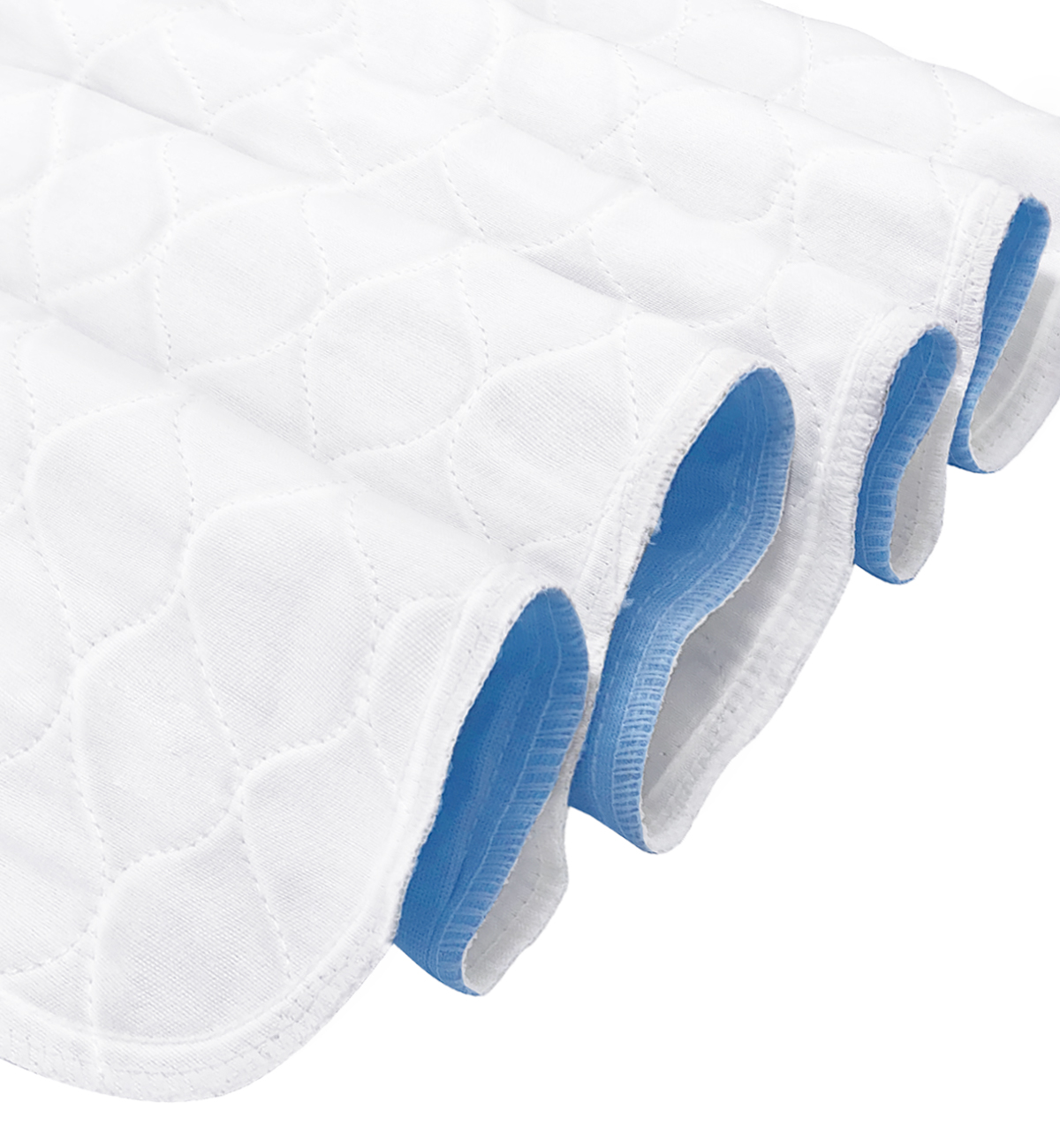
ConkoSil has 5 unique layers enhances absorbent capacity and locks the wound exudate to reduce the risk of skin maceration. The Sacral type is specifically designed for the management of pressure ulcers (bedsores) in the sacral area. Combining advanced silicone technology with innovative foam materials, this dressing provides superior protection and comfort, promoting wound healing and enhancing patient well-being.
To learn more about this tape, visit this website: https://store.conkote.com/product/conkote-ultra-absorbent-silicone-foam-dressing-with-border

Search by Tags
advanced woundcare dressing advanced wound care products Bedsores Blood Blood donation chronic decrease comprehensive guide Conkosil Conkote wound care Diabetes diabetes prevention Diabetes,Foot Problems,wound donation Easy Tips elderly skin care First aid fragile skin dressing gentle wound dressing health life Home Care Ionic Silver Dressin Innovative Technology for Wound Care Lesions Measure a Wound medical tape medical tape for sensitive skin Moist Wound Healing Mouth Taping Negative pressure wound therapy Pressure Ulcers Self-Adhesive Bandage senior wound care silicone foam dressing silicone medical tape Skin care tape traditional wound care dressing Wound care wound care for elderly wound dressing wound healing wound infection wound materials woundmaterials wound type wound vac